Vitamin D Optimization Easiest, Cheapest and Best Strategy to Minimize COVID Infections
STORY AT-A-GLANCE
- Vitamin D optimization is likely the easiest, least expensive and most beneficial strategy that anyone can do to help minimize their risk of infections including COVID-19 coming months
- More than 1 billion individuals worldwide, across all age groups, are deficient in vitamin D, which has now been identified as a significant risk factor for positive COVID-19 status, severe COVID-19 infection and death thereof
- In Indonesia, people with a vitamin D level between 20 ng/mL and 30 ng/mL had a sevenfold higher risk of death than those with a level above 30 ng/mL. Having a level below 20 ng/mL was associated with a 12 times higher risk of death
- To improve your immune function and lower your risk of viral infections, you’ll want to raise your vitamin D to a level between 60 ng/mL and 80 ng/mL (150 nmol/L and 200 nmol/L) by fall
- Vitamin D optimization is particularly important for dark-skinned individuals, as the darker your skin, the more sun exposure you need to raise your vitamin D level, as well as the elderly
All things considered, vitamin D optimization is likely the easiest, least expensive and most beneficial strategy that anyone can do to minimize their risk of COVID-19 and other infections in the coming months. Health authorities are already warning of a second wave of COVID-19 in the fall, which means the time to start addressing your vitamin D level is NOW.
We also have a pandemic of vitamin D deficiency, as more than 1 billion individuals worldwide, across all age groups, are deficient in vitamin D (link, link, link, link). Vitamin D deficiency has now been identified as a significant risk factor for positive COVID-19 status (link, link), severe COVID-19 infection (link, link, link, link) and death (link, link) thereof.
In one study (link, link), which looked at data from 780 hospital patients in Indonesia, those with a vitamin D level between 20 nanograms per milliliter (ng/mL) and 30 ng/mL had a sevenfold higher risk of death than those with a level above 30 ng/mL. Having a level below 20 ng/mL was associated with a 12 times higher risk of death.
To improve your immune function and lower your risk of viral infections, you’ll want to raise your vitamin D to a level between 60 ng/mL and 80 ng/mL by fall. In Europe, the measurements you’re looking for are 150 nmol/L and 200 nmol/L. If vitamin D levels were increased in the global population, tens of thousands of people may be saved if or when COVID-19 reemerges.
While prospective controlled studies demonstrating vitamin D’s effectiveness in COVID-19 are still lacking, there are many such studies underway. You can review the status of these trials on clinicaltrials.gov. As of early June 2020, more than 20 studies had been launched to investigate the benefits of vitamin D against COVID-19.
The Most Important Paper I’ve Ever Written
The comprehensive vitamin D report below has been reviewed by many vitamin D scientists for accuracy. This was done to develop a resource that everyone can share to help educate others. We will soon be launching a campaign to educate and inspire everyone, everywhere, to start optimizing their vitamin D level NOW. Please download my paper here, and share it with everyone you know.
The purpose of this report is to help you understand why it is so important to optimize vitamin levels for healthy immune functions and then provide you with a detailed strategy of how to do that. This report can be used as a tool to teach your friends, family and community about why and how to be prepared for the next pandemic.
In it, I review the science of how your immune system works, and the regulatory role of vitamin D. I also explain how vitamin D reduces your risk of COVID-19 specifically, and how it helps suppress and control both acute respiratory distress syndrome (ARDS) and cytokine storms, which is a primary cause of death in COVID-19.
Darker-Skinned Individuals Need More Vitamin D
Vitamin D optimization is particularly important for dark-skinned individuals, as the darker your skin, the more sun exposure you need to raise your vitamin D level. Increased skin pigmentation reduces the efficacy of UVB because melanin functions as a natural sunblock.
If you’re very dark-skinned, you may need to spend about 1.5 hours a day in the sun to have any noticeable effect. For many working adults and school-age children, this simply isn’t feasible.
Light-skinned individuals may only need 15 minutes of full sun exposure a day, which is far easier to achieve. Still, they too will typically struggle to maintain ideal levels during the winter. During the winter months at latitudes of greater than 40°, little or no UVB radiation reaches the surface of the earth. That said, residence at low latitude does not guarantee adequate vitamin D levels, since social and cultural norms may limit sun exposure.
As noted in the MedCram video above, black, Asian and minority ethnic groups are at an increased risk of death from COVID-19. While some have blamed this racial disparity on health care access, a far more likely reason for this is because dark-skinned individuals are far more likely to be deficient in vitamin D.
In fact, the paper cited by MedCram specifically looked at ethnic disparities in COVID-19 mortality among patients in England, where health care is freely available to all, so the health care access rationale doesn’t seem to hold water.
Vitamin D Supplementation Recommended to Quell Mortality
The role of vitamin D is addressed in a reply by vitamin D researchers William Grant and Barbara Boucher to The BMJ editorial “Is Ethnicity Linked to Incidence or Outcomes of COVID-19?” They write, in part:
“The recent BMJ editorial by Khunti et al. asks ‘Is ethnicity linked to incidence or outcomes of covid-19?’ Here we outline how ethnicity relates to incidence and outcomes of COVID-19 due, in part, to lack of vitamin D because of increased skin pigmentation and diet …
A potentially important factor not considered in the PHE report was vitamin D deficiency, though mounting evidence suggests that vitamin D deficiency is an important risk factor for acute respiratory tract infections and for COVID-19 …
Mounting evidence demonstrates that vitamin D has important roles in regulating the immune system that should reduce COVID-19 risks; primarily by reducing survival and replication of the SARS-CoV-2 virus and by reducing the risks of ‘cytokine storms’ by reducing pro-inflammatory cytokine production and increasing anti-inflammatory cytokine production.
Vitamin D also promotes local ACE2 formation in the lungs, an effect known to reduce the severity of acute respiratory distress syndrome. Furthermore, higher baseline serum 25(OH)D concentrations are currently being reported to be associated with reduced rates of severe COVID-19 and of mortality.”
Grant and Boucher recommend advising the public to supplement vitamin D daily, especially black, Asian and minority ethnic groups, indoor workers, shift workers, the elderly, those in residential care or those confined to their homes, as well as those who are obese. Doing so might reduce COVID-19 severity and prevent unnecessary deaths.
“Vitamin D is readily available … ‘over the counter’ at supermarkets, chemists and online, but could be provided free to those in financial hardship or unable to access supplies,” Grant and Boucher write, adding:
“Doses of 1,000 IU/day in general and of 4,000 IU/day for those at high risk of deficiency, as above, including the BAME groups, should be advised for the duration of the Covid-19 outbreak …”
Sunscreen Advice Counters Lifesaving Vitamin D Message
Remarkably, while the importance of vitamin D against COVID-19 is becoming more widely recognized by doctors, some are still advising against either sun exposure or vitamin D supplementation, or both.
Some, such as Dr. Pieter Cohen, an internal medicine physician at Cambridge Health Alliance in Massachusetts and an associate professor medicine at Harvard Medical School, is even discouraging people from getting their vitamin D level tested to see if they’re deficient! A June 1, 2020, report on Today.com states:
“The body can manufacture vitamin D when the skin is exposed to the sun or get it from food. ‘I’m not making a general recommendation for supplements. I’m saying: To avoid vitamin D deficiency.
It will usually take only being outdoors, getting incidental sun exposure, plus paying attention to the dietary sources of vitamin D,’ [Dr. JoAnn Manson, chief of preventive medicine at Brigham and Women’s Hospital and professor of medicine at Harvard] noted.
Incidental sun exposure means getting some sunshine during a 30-minute walk or other outdoor exercise while wearing shorts or short sleeves (though you should still use sunscreen). It doesn’t mean going out specifically to sun bathe.”
The advice to wear sunscreen while getting “incidental” sun exposure is medically irrational and incorrect, since sunscreen filters out the very ultraviolet rays that trigger vitamin D production in your skin.
In order for sensible sun exposure to work, you need unprotected exposure. Just make sure you don’t get sunburned. All you need is to stay out until your skin turns the lightest shade of pink. After that, cover up with long sleeves and pants.
Help Us Spread the Word!
It is my sincere hope and desire that all of you will help us in this effort to spread the word about vitamin D and get your friends and family on board to get their vitamin levels optimized. We need a citizen army of activists to spread the word. My vitamin D report can help you in this effort. I urge you to share it with everyone you know. I hope to collaborate with all the major natural medical sites to participate in this process.
The vitamin D level you’re aiming for is between 60 ng/mL and 80 ng/mL. In Europe, the measurements you’re looking for are 150 nmol/L and 200 nmol/L. In my vitamin D report, I detail how to go about doing this, but here’s a quick summary of the key steps:
(1) First, measure your vitamin D level — One of the easiest and most cost-effective ways of measuring your vitamin D level is to participate in the GrassrootsHealth’s personalized nutrition project, which includes a vitamin D testing kit.
Once you know what your blood level is, you can assess the dose needed to maintain or improve your level. The easiest way to raise your level is by getting regular, sensible sun exposure, as discussed above.
If you cannot get enough vitamin D from the sun (you can use the DMinder app to see how much vitamin D your body can make depending on your location and other individual factors), then you’ll need an oral supplement. It’s strongly recommended to take magnesium and K2 concomitant with oral vitamin D.
(2) Assess your individualized vitamin D dosage — To do that, you can either use the chart below, or use GrassrootsHealth’s Vitamin D*calculator. To convert ng/mL into the European measurement (nmol/L), simply multiply the ng/mL measurement by 2.5. To calculate how much vitamin D you may be getting from regular sun exposure in addition to your supplemental intake, use the DMinder app.
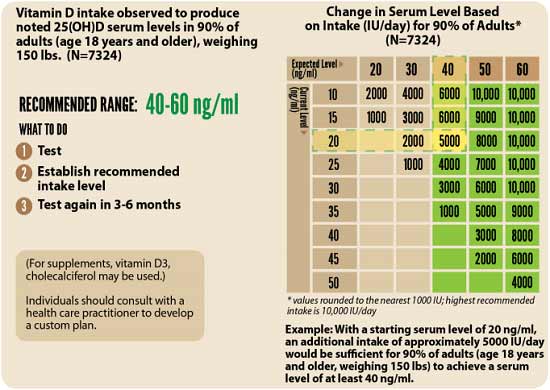
(3) Retest in three to six months — Lastly, you’ll need to remeasure your vitamin D level in three to six months, to evaluate how your sun exposure and/or supplement dose is working for you.